Keratoconus Explained
Published by on September 22, 2015
Our eyes are precious and taking care of them should be a top priority. It’s hard to recognize early signs of particular eye conditions without the help of a specialist. One eye condition many people are unaware of is Keratoconus. For those of you who haven’t heard of this before, we at Kugler Vision in Omaha, NE have information for you about this eye condition.
What is Keratoconus?
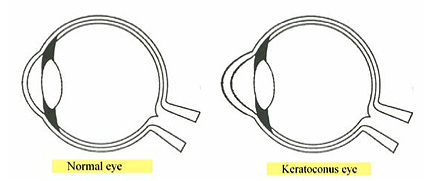
Keratoconus is a vision disorder that occurs when the normally round, dome-shaped cornea progressively thins. This thinning causes a cone-like bulge to develop. Due to the change in shape of the cornea, Keratoconus most often leads to significant distortion in vision– with a notable reduction in the sharpness of vision (visual acuity). This impairment in vision can severely affect a keratoconus patient’s life by making even simple daily tasks difficult to perform. Some of these affected tasks are:
- driving
- watching television
- reading a book
Why does Keratoconus occur? When is it detected?
The actual cause of keratoconus is not yet know, but there have been studies that suggest a genetic link to the disease. The disease typically affects both eyes, but they may not be affected evenly or at the same rate. Keratoconus is usually detected in a person’s adolescent years. It is somewhat rarer to be detected late in life. That is why it is important to talk with your teenagers and ask them if they are experiencing any strange changes in their sight. You should also take them for eye examinations and checkups regularly.
How are Keratoconus symptoms treated?
Glasses or soft contact lenses may be used to correct the mild nearsightedness and astigmatism that result from the early stages of keratoconus. As the disease progresses and the cornea continues to thin and change shape, rigid gas permeable (RGP) lenses are often prescribed because glasses and soft contact lenses are no longer adequate to correct one’s vision.
The RGP lenses must be carefully fitted and frequent checkups and lens changes are often required to continue to achieve good vision. However, more issues may develop over time for the Keratoconus patient wearing RGP lenses. These issues include:
- the cornea may become scarred
- the contact lenses may no longer be comfortable to wear on a daily basis
- and/or the contact lenses may no longer be able to adequately correct vision.
In severe cases of keratoconus, the doctor may recommend the patient have a corneal transplant treatment, also known as a penetrating keratoplasty procedure (PKP). A transplant would be needed because of corneal scarring, corneal thinning, or the inability to wear contact lenses. A corneal transplant procedure involves removing the patient’s cornea and replacing it with healthy corneal tissue from a donor. Most patients will still need to wear glasses or contact lenses for clear vision following a corneal transplant. Until now, when RGP lenses are no longer effective or have become uncomfortable to wear on a daily basis, a corneal transplant has been a Keratoconus patient’s only option to attempt to restore their visual acuity. INTACS inserts may offer an alternative to restore functional vision and potentially to defer the need for a corneal transplant procedure. They are two small, plastic crescents or arcs, which are designed to remain permanently in the eye. A recent study that appeared in the Journal of Refractive Surgery concluded that 92.9% of eyes with progressive keratoconus did not progress after INTACS were implanted.
Benefits of INTACS
- improves vision and allows a more successful contact lens fit
- reduce the nearsightedness and astigmatism associated with keratoconus
- preserve the central part of the cornea which is most important for vision
- defer the need for a corneal transplant procedure
- can be surgically removed or replaced

Lance Kugler, MD, is a specialist in LASIK and vision correction surgery and CEO of Kugler Vision. A proud Omaha native, he is passionate about improving lives through clear vision. Dr. Kugler serves on several national boards, and his practice is recognized internationally as a center of excellence. Dr. Kugler is one of the original founders of the Refractive Surgery Alliance, an international organization comprised of over 350 of the world’s leading vision correction surgeons; he also served as its first president. In 2019, Dr. Kugler was selected as a TEDx speaker, and delivered a talk in Omaha about the worldwide epidemic of nearsightedness and refractive solutions. Dr. Kugler is an Associate Professor of Refractive Surgery at the University of Nebraska Medical Center’s Truhlsen Eye Institute, has been published in many medical journals, and participates in numerous clinical studies to advance the field of vision correction surgery. Additionally, Dr. Kugler is proud to be a Board Certified Fellow of the World College of Refractive Surgery & Visual Sciences. Dr. Kugler and his wife are proud parents to five active kids. When he has a spare moment, he enjoys skiing, tennis, travel, and fine coffee.
Leave a Reply